Disease details
Hydrosalpinx: Detailed Information
Hydrosalpinx is a condition where a fallopian tube is blocked with a watery fluid. The term originates from “hydro” (water) and “salpinx” (tube). This blockage can affect one or both fallopian tubes, leading to complications, particularly with fertility.
Causes
Hydrosalpinx typically results from the following causes:
- Infections: Pelvic inflammatory disease (PID) is a common cause, often resulting from sexually transmitted infections (STIs) like chlamydia or gonorrhea.
- Previous Surgery: Past abdominal or pelvic surgeries can lead to adhesions and subsequent blockage of the fallopian tubes.
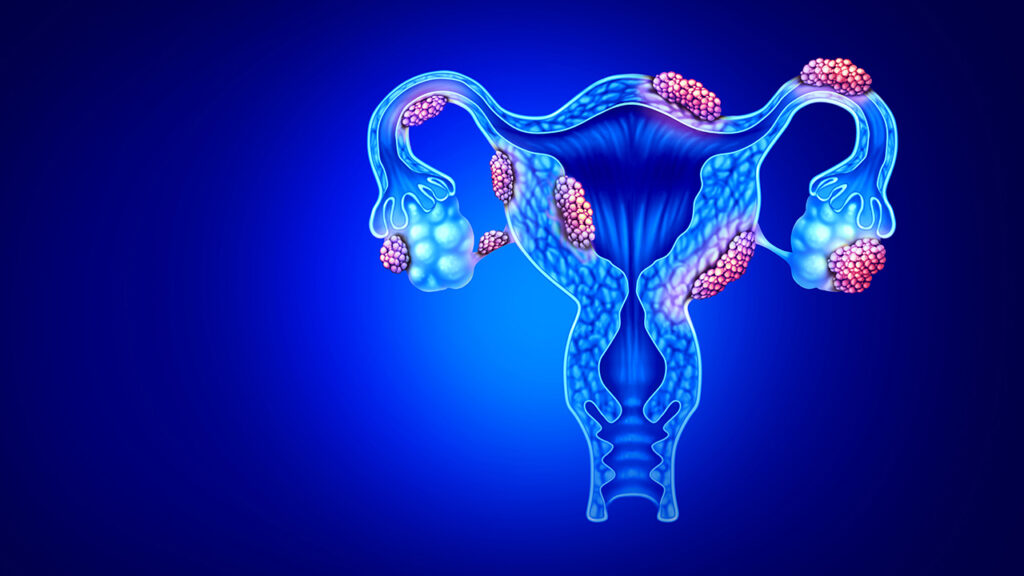
- Endometriosis: The growth of endometrial tissue outside the uterus can cause scarring and blockage of the fallopian tubes.
- Tuberculosis: Genital tuberculosis is a significant cause in certain regions.
- Congenital Anomalies: Rarely, congenital issues can lead to blocked fallopian tubes.
Symptoms
Hydrosalpinx can often be asymptomatic, meaning many women do not experience noticeable symptoms. When symptoms do occur, they may include:
- Chronic pelvic pain or discomfort.
- Abnormal vaginal discharge.
- Menstrual irregularities.
- Pain during intercourse.
- Infertility, as blocked fallopian tubes can prevent sperm from reaching the egg or the fertilized egg from reaching the uterus.
Diagnosis
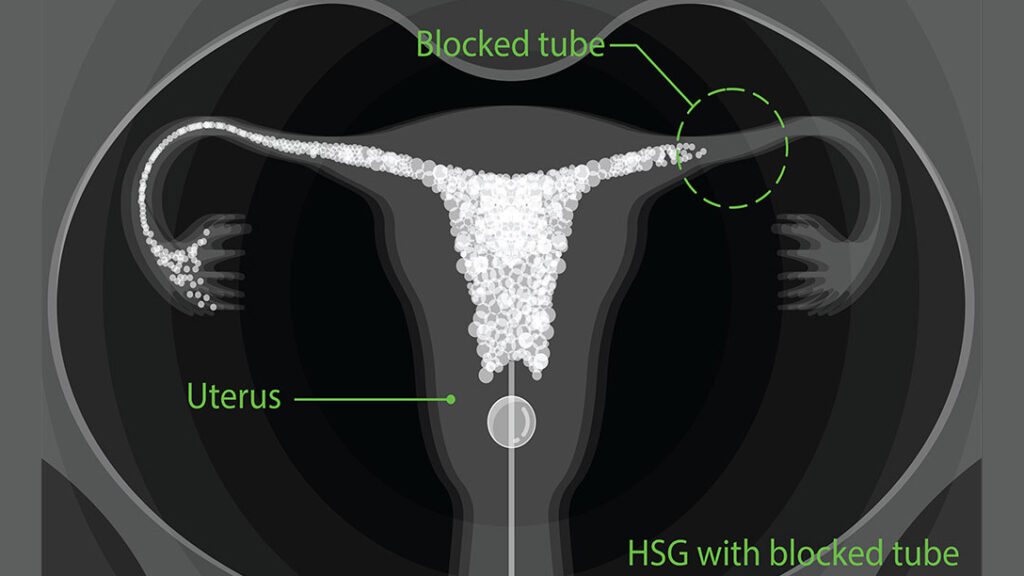
Hydrosalpinx is typically diagnosed using imaging techniques and tests such as:
- Hysterosalpingography (HSG): An X-ray test where dye is injected into the uterus and fallopian tubes to check for blockages.
- Ultrasound: Can show the presence of fluid-filled tubes.
- Laparoscopy: A minimally invasive surgical procedure allowing direct visualization of the fallopian tubes.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the reproductive organs.
Treatment
The treatment for hydrosalpinx depends on various factors including the severity of the condition, the desire for future fertility, and the underlying cause. Common treatments include:
- Antibiotics: If an infection is present, antibiotics may be prescribed.
- Surgical Intervention:
- Salpingostomy: Creating an opening in the fallopian tube to drain the fluid.
- Salpingectomy: Removal of the affected fallopian tube(s), often recommended if IVF is planned, as the fluid can negatively affect implantation.
- Tubal Ligation Reversal: In cases where previous sterilization surgery is the cause.
- In Vitro Fertilization (IVF): Often recommended if natural conception is challenging due to hydrosalpinx. Removing or blocking the damaged tubes before IVF can improve success rates.
Prognosis
The prognosis for hydrosalpinx largely depends on the treatment chosen and the extent of the damage. Surgical removal or correction of the affected tube(s) often results in good outcomes, especially when followed by fertility treatments like IVF.
Complications
If left untreated, hydrosalpinx can lead to:
- Chronic pelvic pain.
- Ongoing infections.
- Increased risk of ectopic pregnancy.
- Infertility issues.
Prevention
Preventive measures include:
- Regular screening and prompt treatment of STIs.
- Practicing safe sex to reduce the risk of infections.
- Early treatment of pelvic infections to prevent progression to PID.
- Regular gynecological check-ups, especially if experiencing symptoms related to reproductive health.
Hydrosalpinx can significantly impact a woman’s reproductive health and overall well-being. Early diagnosis and appropriate treatment are crucial in managing this condition and improving fertility outcomes.
Elongated uterus: Detailed Information
An elongated uterus is a condition where the uterus is longer than the typical size. This term may describe an anatomical variation or be associated with certain medical conditions. Below is a detailed overview of the elongated uterus, including potential causes, symptoms, diagnosis, treatment, and implications.
Anatomy of the Uterus
The uterus is a pear-shaped organ in the female reproductive system. Its typical dimensions are approximately 7.5 cm in length, 5 cm in width, and 2.5 cm in thickness. Any significant deviation from these dimensions, particularly an increase in length, may be referred to as an elongated uterus.
Causes of Elongated Uterus
- Congenital Factors: Some women may be born with an elongated uterus due to genetic variations.
- Hormonal Influences: Hormonal imbalances, particularly involving estrogen, can lead to changes in uterine size and shape.
- Fibroids: Benign tumors known as fibroids can cause the uterus to enlarge and elongate.
- Adenomyosis: A condition where the inner lining of the uterus breaks through the muscle wall of the uterus, leading to an increase in size.
- Endometriosis: The presence of endometrial tissue outside the uterus can cause adhesions and elongation.
- Uterine Polyps: These growths can alter the shape and size of the uterus.
- Pregnancy and Childbirth: Multiple pregnancies and deliveries can lead to changes in uterine size and shape.
- Pelvic Inflammatory Disease (PID): Chronic inflammation can cause structural changes in the uterus.
Symptoms
An elongated uterus may be asymptomatic in many cases. When symptoms do occur, they can include:
- Pelvic pain or discomfort.
- Abnormal menstrual bleeding, such as heavy or prolonged periods.
- Pain during intercourse.
- Lower back pain.
- Urinary frequency or urgency if the elongated uterus presses on the bladder.
- Infertility or difficulty conceiving.
Diagnosis
Diagnosis of an elongated uterus typically involves:
- Pelvic Examination: A physical examination can sometimes reveal an enlarged uterus.
- Ultrasound: A transvaginal or abdominal ultrasound can provide detailed images of the uterus.
- MRI or CT Scan: Advanced imaging techniques can offer more precise measurements and identify underlying conditions.
- Hysteroscopy: A procedure using a thin, lighted tube to look inside the uterus.
- Laparoscopy: A minimally invasive surgery to view the pelvic organs.
Treatment
Treatment for an elongated uterus depends on the underlying cause and the severity of symptoms. Options include:
- Medications:
- Hormonal treatments, such as birth control pills or hormone therapy, to regulate menstrual cycles and reduce symptoms.
- Pain relievers for managing discomfort.
- Medications to shrink fibroids or manage adenomyosis.
- Surgical Interventions:
- Myomectomy: Removal of fibroids while preserving the uterus.
- Hysterectomy: Removal of the uterus, typically recommended for severe cases or when other treatments have failed.
- Endometrial Ablation: Removal of the uterine lining to reduce bleeding.
- Laparoscopic Surgery: To treat conditions like endometriosis.
- Lifestyle and Alternative Treatments:
- Dietary changes and exercise to manage symptoms.
- Acupuncture or other complementary therapies for pain relief.
Implications
An elongated uterus can have several implications, particularly concerning reproductive health:
- Fertility Issues: Structural changes in the uterus can impact conception and pregnancy.
- Pregnancy Complications: Increased risk of miscarriage, preterm labor, and delivery complications.
- Chronic Pain: Persistent pelvic pain and discomfort can affect quality of life.
- Menstrual Irregularities: Heavy or prolonged periods can lead to anemia and fatigue.
Prevention and Management
While congenital factors cannot be prevented, managing the risk factors and early treatment of underlying conditions can help:
- Regular gynecological check-ups to monitor uterine health.
- Prompt treatment of infections and inflammatory conditions.
- Hormonal balance through lifestyle modifications and medical management.
- Awareness of family history and early intervention for genetic conditions.
Understanding the causes and implications of an elongated uterus is crucial for effective management and treatment. Early diagnosis and appropriate medical care can significantly improve outcomes and quality of life for those affected by this condition.
